A new study published in the Journal of Neuroinflammation, by Professor Marc Ruitenberg and his research team at The University of Queensland, has yielded important insights about the effect of a spinal cord injury (SCI) on the body’s immune system, and how this impacts recovery. SpinalCure caught up with Prof Ruitenberg to discuss these latest findings.
 Prof Ruitenberg (left) and members of his team with Duncan Wallace
Prof Ruitenberg (left) and members of his team with Duncan Wallace
The aim of the new research (which was conducted in vivo via special mouse models) was to expand on the group’s extensive knowledge of the inflammatory response following an SCI. This response is known to exacerbate spinal cord tissue damage, and thereby can significantly worsen patient outcomes. However, there is also evidence that the immune system as a whole may be weakened by an SCI. A key aspect of Prof Ruitenberg’s research centres on understanding this paradox better.
The published article: Single-cell RNA sequencing reveals peripheral blood leukocyte responses to spinal cord injury in mice with humanised immune systems. Journal of Neuroinflammation. https://doi.org/10.1186/s12974-024-03048-0
“What we know is that people with an SCI, particularly a high-level one, often have a weakened immune system,” explained Prof Ruitenberg. “Particularly, early on, many SCI patients often suffer from pneumonias or other sorts of infectious complications that can be life threatening, see them end up in ICU, or have their stay in ICU prolonged. What we also know is that an infection has the potential to negatively interfere with recovery because of the way it activates the immune system.”
“However, what we didn’t fully know is how one’s immune system is impacted after an SCI at a deeper cellular and molecular level. Another question that we certainly cannot answer in patients is what happens when a human immune cell leaves the blood and enters the lesion site at the core of a spinal cord injury,” he added.
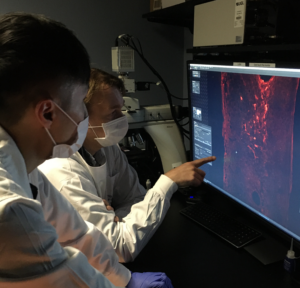
To address these questions, the new study tested three experimental groups of animals: normal mice, immunocompromised mice without an immune system, and so-called humanised mice that had been given a human immune system. A key result here was that, when subjected to an SCI, the group without an immune system had a much better recovery; the introduction of human immune cells annulled this effect. These findings confirmed the net detrimental role that immune activation and/or inflammation plays in recovery from SCI. Prof Ruitenberg and his team then analysed immune cell responses at the very deep molecular level by using single-cell RNA sequencing.
They first compared human immune cells isolated from the blood of healthy controls sham-operated controls (mice that were subjected to surgery and had damage to the vertebral column but not spinal cord), or SCI subjects.
“This really gave us an unprecedented insight in terms of how these immune cells are functionally changed by SCI in an adverse way. The next phase of that research will now explore ways to try and revert this phenomenon so they’re responding in a normal way and to then test whether this will have a positive impact in terms of recovery and the incidence of adverse infectious complications early-on,” Prof Ruitenberg explained.
By isolating human immune cells also from the injured spinal cord, they gained unprecedented insights as to how these cells are behaving at the lesion site itself.
“The sequencing work gave us a profile of all the molecules these cells start to express and regulate once they enter the lesion side. Through that process, we’ve been able to identify a whole suite of immune-related genes and pathways that we think might be driving some of the harmful inflammation that causes further pathology and additional loss of otherwise healthy spinal cord tissue. So, going forward, what we really want to do now is start to manipulate these genes and see whether this improves outcomes for SCI,” he continued.
Prof Ruitenberg said that the study has the potential to support a cure for SCI from a recovery perspective in the scheme of his wider work.
“Ultimately, what we really want to do is minimise the damage that is occurring to the spinal cord after injury. This body of work enables us to analyse how immune cells might be contributing to that, and ultimately how the immune system may be manipulated to support regeneration instead, as it does in other healing tissues, rather than being a negative factor that is making things worse when a person presents with a spinal trauma in the acute phase of SCI,” he added.
“An important application of humanised mouse models, from a translational perspective, is that they provide an opportunity to directly study human immune cells and how these cells respond to specific drugs may be beneficial for treating SCI.”
These new findings are set to contribute to the ongoing preclinical work that is supported by SpinalCure as to how intravenous immunoglobulin, an immunomodulatory therapy that Prof Ruitenberg and his collaborators brought to a world-first clinical trial, may act to improve recovery from SCI.